 Natural sciences
Natural sciences
How does the coronavirus mutate?
In spring, the neurological symptoms in patients with COVID-19 such as the loss of smell or taste were scarce. They appeared much more seldom than problems with respiration or high fever. Now, the loss of smell or taste practically defines the coronavirus.
Medical doctors begin the medical history examination of a patient with a question "Have you lost smell or taste?" More and more patients complain about having problems with memory, concentration or collecting their thoughts. New questions are appearing if the coronavirus has mutated since last spring and if it has begun to cause other symptoms or is it rather the patients themselves who have started paying attention to other symptoms of the disease. The answer to this question is very simple. The virus SARS-CoV-2 mutates as any other virus, but it does so more slowly than the virus of influenza of HIV. All mutations which appear in the coronavirus are monitored globally and almost in their real time, and displayed in GISAID database. This database was initially set up to monitor such viruses as avian influenza, but recently it is effectively used as a database to run research on SARS-CoV-2.
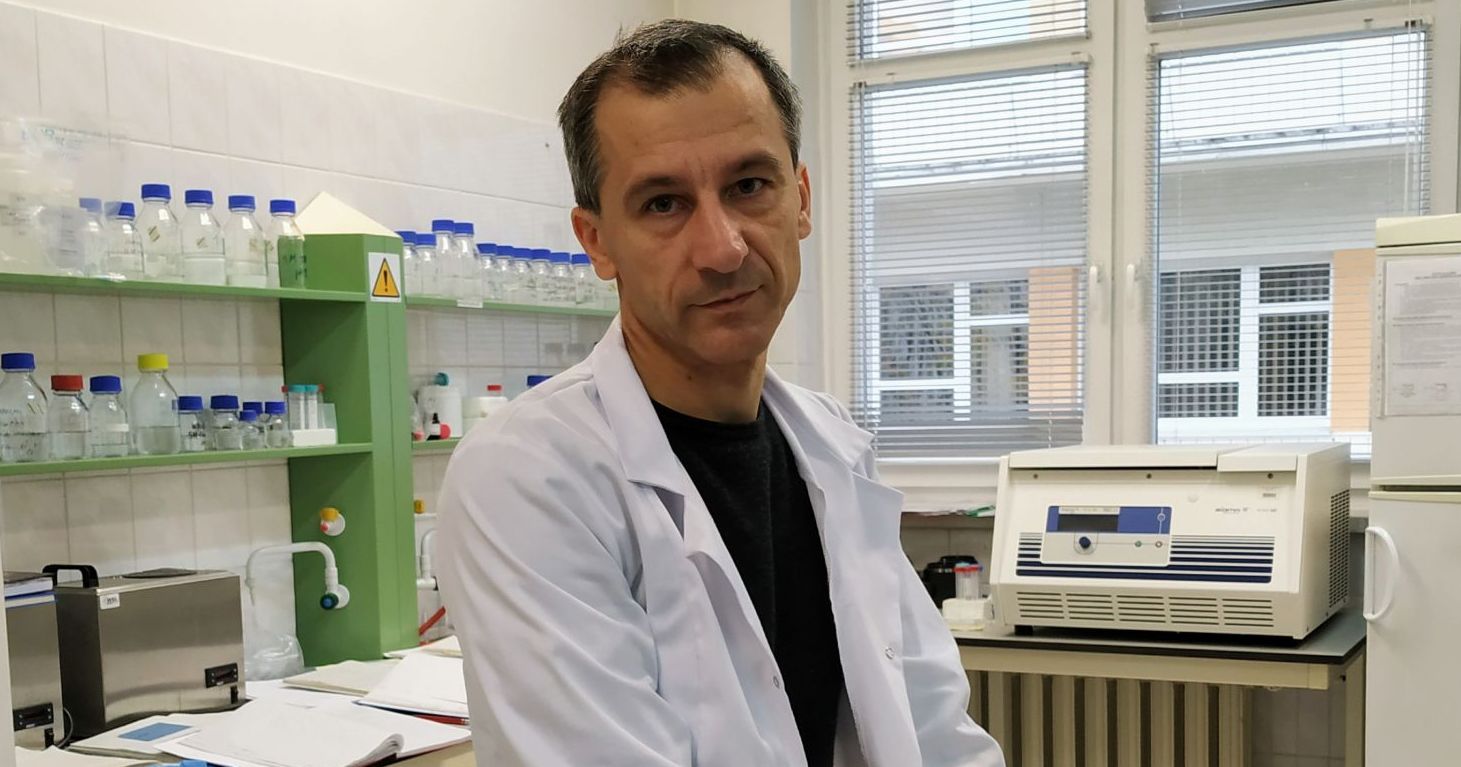
So far, after sequencing over 200 thousand genomes of the virus, several thousand mutations of SARS-CoV-2 have been identified – says Rafał Butoft, Dr. habil, NCU professor from the Chair of Normal Anatomy in Collegium Medicum, NCU. – This is a huge number considering that the virus contains the RNA genome of the size of 29 thousand nucleotides. Still, most of those mutations are either neutral of harmful for the virus itself, and therefore they do not remain too long in the virus population.
Scientists underline that a new mutation in the virus is relatively easy to identify. More difficult it is to establish its phenotype role for the virus. So far, only one mutation in SARS-CoV-2 has been convincingly characterized. In May, a group of scientists from Los Alamos under the supervision of an American biologist Bette Korber issued a joint study. It showed that the mutation in amino acid in the position 614 of a protein S (spike protein on the surface of the virus), in which instead of amino acid D appears amino acid G, increases infectivity and the capability of transmission, but does not increase the severity of symptoms of COVID-19.
The research was published in the journal "Cell" and its results were confirmed in many other research centers. – After a discussion with the scientists from Los Alamos over this mutation, which is named D614G, we had a conceptual work published. Our intention was to advocate that this mutation may contribute to higher frequency of smell disorders in COVID-19 among people from Europe and America in comparison with the inhabitants of East Asia (Butowt, Bilińska i von Bartheld, 2020, ACS Chem Neuroscience) – explains the scientist from CM NCU. – D614G mutation helps the virus to penetrate through the cells of olfactory epithelium, and thus it may increase the probability of anosmia. Practically, no other mutation out of those several thousand mutations in SARS-Cov-2 but this one has been so thoroughly and convincingly examined. We do know mutations which appear spontaneously and disappear quickly such as, for instance, deletion of 382 nucleotides in SARS-Cov-2 genome region described as Orf8. This mutation appears and disappears without causing a selective advantage to the virus. On the contrary, it makes it weaker and does causes lighter symptoms of COVID-19 among the patients infected.
Similar phenomenon happens in other mutations which do not give any advantage to the mutated virus. It was different with the mutation D614G, described above, which has sustained and now dominates almost in the whole world. Sometimes, however, other mutations may appear which will sustain in the population of SARS-Co-2 for a longer period of time. In Europe last summer, for example, a strain of SARS-CoV-2 was described as one having a group of a few mutations, among which there were A222V in protein S and A220V in the protein of nucleocapsid, and a few other coexisting alterations in the genome. The occurrence of this virus is limited only to the territory of Europe. For the time being, it is unknown whether this group of mutations offers any advantage to the viruses that transmit it. In general, we have no hard evidence that mutations in SARS-CoV-2 have increased the infectivity of the virus or have affected the severity of the symptoms of COVID-19. It has not been demonstrated that any mutation of coronavirus existing in a human endangers the preparation process of vaccines. On the contrary, it has been demonstrated that the mutation D614G increases the fixation of antibodies with the virus protein S. It seems that mutations that endanger the effectiveness of vaccines may still appear in bigger numbers at the moment of selective pressure, which is after the application of a given vaccine on a large scale.
- This is why the Danish' decision to kill about 17 million of farmed minks because of a new mutation of the virus SARS-CoV-2 existing in the population of this virus among these animals remains very controversial. In my opinion, such a step is rather unreasonable – says professor Butoft.
- This is why the Danish' decision to kill about 17 million of farmed minks because of a new mutation of the virus SARS-CoV-2 existing in the population of this virus among these animals remains very controversial. In my opinion, such a step is rather unreasonable – says professor Butoft. – This mutation gives the virus an advantage in fixating to the receptor ACE2 in minks, but it does not affect the fixation to ACE2 receptor in human., thus it should not sustain in the virus existing in the human population. The Danish argue they have discovered cases in which the virus has been transferred with the new mutation from minks to people. Indeed, it is possible, but such cases will remain incidental, rather limited to those who work with these animals. Chances that such a virus will spread on a large scale among people are scarce because, as I mentioned, the mutation which is advantageous for the virus among minks does not give any selective advantage among people dure to tiny differences in the structure of receptor ACE2 in minks and humans.
Back to disorders of the sense of smell, they are now the basis of isolating people even if other symptoms of COVID-19 are absent. This is why, for a few months in a few parts of the world, scientist is attempting to construct simple devices to measure the smell among people, based on applications of a few or more olfactory substances in aerosol, and not based on strips of filter paper saturated with such substances. This method is more sensitive and there are already results which show that 90% of people infected with SARS-CoV-2 and tested in this way exhibit some degree of smell disorders, which sometimes they may not even be aware of.
- Yet, we still do not know many things and a lot of issues make a new and intriguing area of research – points out professor Butoft. – A very interesting and still unsolved question is why some patients demonstrate a complete loss of smell whereas others almost do not experience it. It is very likely that the research on disorders of smell during COVID-19 will help explain a fundamental problem why this disease proceeds so differently in various patients. For the time being, we lack convincing and confident evidence that this is only the issue of differences in the response of the immune system in particular people.
What still needs explaining is the issue of the virus penetrating into the brain through the olfactory system. A lot of researchers claim at the moment that there is no credible evidence that this is the way in which infection occurs, at least among a significant number of patients. Of course, there exist data which show the presence of SARS-CoV-2 virus in olfactory neurons and brain neurons in the research material from people who died of COVID-19. Still, it must be remembered that these cases are very unique as, before death, a lot of life functions of many organs break down, including the damage of the blood-brain barrier as the virus may move practically everywhere during the last hours preceding death. This, however, does not refer to the majority of patients. – On the other hand, however, a lot of research work indicates the presence of the virus in the cerebral spinal fluid in living patients, and it is still not known how it is transferred there – says the scientist from Bydgoszcz. – Other questions which need answering and stem from the intriguing loss of smell during COVID-19 are, for example, why these disorders hardly occur in elderly people and those from East Asia in comparison to Europeans.
 NCU News
NCU News






 Natural sciences
Natural sciences
 Natural sciences
Natural sciences